ΩΡΛ ΑΘΗΝΑΣ : ΔΙΕΘΝΕΙΣ ΔΗΜΟΣΙΕΥΣΕΙΣ – ΑΝΑΚΟΙΝΩΣΕΙΣ & ΑΡΘΡΑ
Ο Δρ. Γεώργιος Μοιρέας είναι Χειρουργός Ωτορινολαρυγγολόγος με Εξειδίκευση στη Ρινοπλαστική και Πλαστική Χειρουργική προσώπου.
 ΠΑΓΚΟΣΜΙΑ ΚΑΙ ΠΑΝΕΥΡΩΠΑΙΚΑ ΣΥΝΕΔΡΙΑ
ΠΑΓΚΟΣΜΙΑ ΚΑΙ ΠΑΝΕΥΡΩΠΑΙΚΑ ΣΥΝΕΔΡΙΑ
Ο χειρουργός Ωτορινολαρυγγολόγος Γεώργιος Μοιρέας και η συμμετοχή του σε παγκόσμια & πανευρωπαικά συνέδρια :
7th Annual Meeting of the Rhinoplasty Society of Europe & 6th Bergamo Open Rhinoplasty Course. 14-17 Μαρτίου 2018.. Pappa Giovanni XXIII Congress Center, Bergamo, Italy
A Triple-Hit Technique to manage Bifid Tip Deformity
Mireas George1,2, Katsouli Georgia3
Introduction
Bifid tip is the result of strong Lower Lateral Cartilages (LLCs) covered by relatively thin skin and soft tissue envelope causing a particular appearance of a wide nasal tip often disproportional in width with the nasal dorsum.
Numerous different surgical techniques have been described to meet this challenge leading to various results and often complications.
Complications
The major problem of bifid-tip surgeries is the LLC’s over-rejection combined with the unpredictable shrinking at the scroll area and caudal alar rim.
Most common complications are bossa formation, tip asymmetries and scroll-area pinching.
The goal
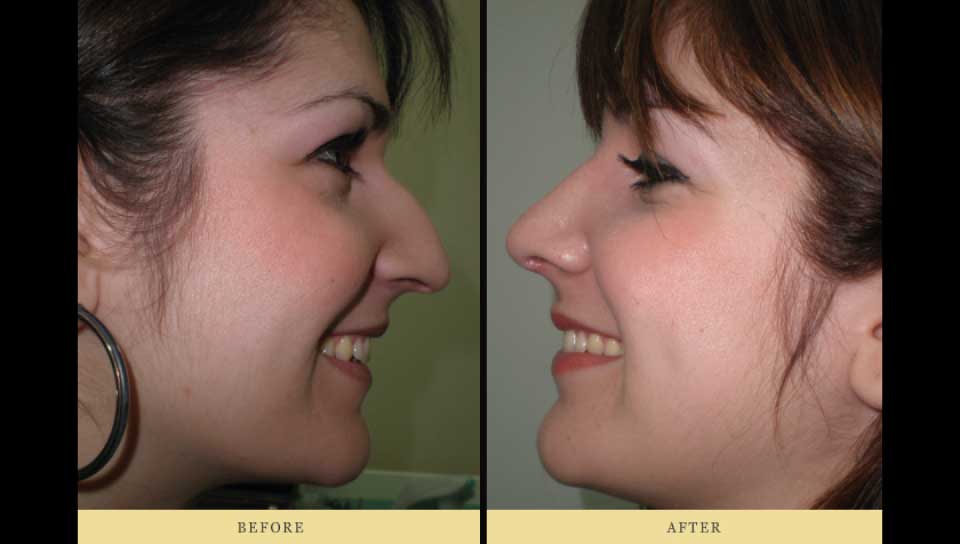
Our scope was to achieve a narrower nasal tip, with symmetrical tip defining points and natural appearance.
At the same time we had to avoid over and under-correction along with the unpredictable shrinking especially at the cephalic and caudal area of LLCs.
The Triple-Hit Technique
- Managing LLC dimensions with “Stripe-out middle & Slide cephalic LLC”
In order to manage the volume of LLCs and avoid cephalic trimming and potential pinch distortion within scroll region we create a Stripe-out of the middle part of LLCs continued by sliding of the cephalic under the caudal part totally preserving the scroll area.
The removed cartilage is a stripe 2-6 mm mostly parallel to the longitudinal axis of the LLC corpus extending till the outer border of the LLC in order to create two totally separated divisions of the LLC without any disruption of the anatomical integrity of the scrool region. The upper part is sliding downwards and sutured (5.0 PDS) under (rarely over) the lower part creating a new LLC which is completely manageable, with measurable dimensions and natural cephalic and caudal borders. The stripe depending on each case can be from parallelogram to wedge-shaped and identical or not at both sides.
An alternative to sliding is to rotate (inwards or outwards) the cephalic part especially in cases we want to alter the concavity/convexity of the lateral alar cartilage.
- Managing LLC rotation and tip contouring with CTS
We are using Cranial Tip Suture to obtain proper eversion of the caudal alar rim and avoid pinching.
Combining CTS with a strong but well-defined LLC as described above protects us from alar rim buckling inward and unnatural appearance.
- Managing Tripod stability and symmetry with SEG or Col Strut
The new LLCs are anchored to a Septal Extended Graft or a Columella Strut to achieve constant and proper support and symmetry.
For final contouring the entire construction is furthermore manageable with the use of a suture between the middle of the cephalic borders of our new LLCs to decrease the overall width of the new tip along with equalizer sutures and/or small tip-grafts.
Discussion – Conclusion
Bifid-tip rhinoplasties could lead to unpredictable shrinking causing asymmetries and pinching at scroll area or alar rim while the fear of that could lead to severe under-correction of the bifidity.
Maintaining the anatomical integrity of the scroll region, controlling the dimensions and orientation of our new LLCs along with tripod securing can prevent these complications.
The Triple-Hit seems to be a reliable All-in-one Technique in creating a constant, well-defined symmetrical tripod and a nasal tip with natural appearance, non-vulnerable to shrinking and deviations.
Annual Conference of European Academy of Facial Plastic Surgery, 27-30 Σεπτεμβρίου 2017Altis Grand Hotel, Lisboa, Portugal
Ιnverted papilloma of nasal septum. A rare case of revision surgery.
George Mireas1,2,3; Georgia Katsouli1,2
Background
Inverted papillomas represent one of the 3 distinct histomorphologic types of the uncommon benign sinonasal tumors called Schneiderian papillomas. Inverted papillomas commonly occur in males aged 40-70, they arise from the lateral nasal wall near the middle turbinate and extend into the sinuses. In extremely rare cases they arise from the nasal septum. Most common symptoms are nasal obstruction, epistaxis and anosmia. Surgical excision is the best treatment.
History
Male patient, aged 56, with severe obstruction and epistaxis of left nostril caused by a mass deriving from septum.The patient reported 5-years history with a cauterization 1y after first appearance and a surgical excision 2y ago. Direct endoscopy of nose, pharynx, mouth and larynx was free of pathological findings.
Surgical approach
Modified lateral rhinotomy incision was chosen because it causes minimal functional and esthetic deformity and provides excellent exposure of the lower part of the nasal cavity and the septum.Externally the incision started at nostril sill and was extended around the alar base and lobule, through the alar-facial junction to end at the middle of the nasolabial crease.Internally the incision was carefully placed above the mass.
Mass excision
A typical hemi-transfixion incision was made, which followed by unilateral septal mucoperichondrium elevation. The elevation continued downwards to nostril floor and a deep surgical plane under the mass was made with an outward rotation. The deep plane extended laterally till the lateral modified rhinotomy incision and the mass were excised in one single piece measured approx. 30*20*5 mm.
Defect closure
A defect about 30*15 mm has been made on the one side of the septum, while the caudal nostril floor was totally removed along with the lower portion of the lateral side wall. A full-thickness nasolabial flap was elevated and rotated to cover the surgical defect. With the flap in place and the lateral wall moved to its natural position a small portion of the flap was then superficially trimmed just to avoid having overlapping with the skin in the middle.Flap’s inner portion that covered septum and nostril’s floor was fixed in place while it’s outer portion was appropriately trimmed and closed in layers. The lateral wall was turned back and fixed to its normal position. Interrupted vicryl 4.0, PDS 5.0 and nylon 6.0 sutures were used for flap’s fixation and rhinotomy closure. A silastic splint was inserted for one week to support and tamponade the graft.
Results
Histopathology report revealed Inverted nasal papilloma with specimen’s edges without invasion. Patient’s nose breathing ability returned to normal just a few days after surgery, while his postoperative appearance showed a well-healed scar without esthetic deformity especially 6m after surgery. Observation for 3.5 years with full rhinolaryggoscopy every six months did not show any recurrence of the disease.
Annual Conference of European Academy of Facial Plastic Surgery, 27-30 Σεπτεμβρίου 2017 Altis Grand Hotel, Lisboa, Portugal
Vectra 3D/M3 Imaging System for Rhinoplasty and Chin plastic surgery. Evaluation of 3D Simulation system in Pre-op consultation.
George Mireas1,2,3; Georgia Katsouli1,2
Purpose
Evaluation of 3D Imaging and Surgery Simulation in pre-op consultation for Rhinoplasty and Chin surgery.
Materials and Methods
We used Vectra 3D/M3 Imaging system for a period of 8 years in more than 1000 patients (male:female 1.5:2, age:16 – 70) interested on rhinoplasty and/or chin surgery.
The system consists of :
a. The Vectra 3D/M3 (Canfield Scientific) capture system
b. A Computer
c. Mirror and Face Sculptor software for Analyzing 3D images and making 3D simulation of surgical procedures of Face and Neck
The simulation process starts by capturing the patient’s three-dimensional image with the VECTRA 3D, which takes about a minute.
The system has 6 cameras positioned in pairs in a triangle base.
After capturing these 6 views the Vectra’s image processing software finally computes a highly accurate map of three-dimensional shape and color coordinate of the observed surface.The 3D image is fully customizable by the surgeon during the surgery simulation
The standard procedure during all pre-op consultations was the following: 1. Taking history and clinical evaluation
2. Endoscopy of the nose
3. 3D image capture
4. 3D surgery simulation and discussion
Results
3D imaging and surgery simulation has benefits categorized into 2 distinct groups: A. Technical Advantages
1. 3D image capture in less than 1 minute.
2. Post-op simulation from altering and differing angles.
3. Showing pre-op and post-op images side by side 4. Measuring distances
5. Measuring volumes
6. Viewing 2 different angles
7. Combination of 2 or more surgical procedures
8. Comparison of 2 rhinoplasty +/- chin surgery versions
9. Printing surgery result from 1 to 6 different angles
B. Communication Advantages
1. Simplifies the communication between patient and surgeon.
2. Eliminates the misunderstandings about the expected surgery results
3. Decreases patient’s stress
4. Patient’s decision is faster and more solid
Concerning the disadvantages of using a 3D simulator, one could mention the cost of buying such a system which is a little bit high but on the other hand keeping in mind that the procedure itself doesn’t have any cost.
Conclusion
3D simulation during Rhinoplasty and Chin surgery consultation is a powerful tool in the hands of a qualified surgeon. It gives many technical pre-op possibilities to the surgeon and great advantages to the patient-surgeon communication.
The Journal of Laryngology & Otology (2006), 120, 298–304.
IMMUNOHISTOCHEMICAL DETECTION OF E-CADHERIN IN CERTAIN TYPES OF SALIVARY GLAND TUMOURS
1Andreadis DS, DDS, PHD, 1Epivatianos ADDS, PHD, 2Mireas G, MD, 3Nomikos A, MD,
1Poulopoulos A, DDS, MSC, PHD, 4 Yiotakis J, MD, 3Barbatis C, MD, FRCPATH
1Department of Oral Medicine and Maxillofacial Pathology, Dental School, Aristotle University of Thessaloniki,Thessaloniki, the Departments of 2ENT Surgery and 3Histopathology, Red Cross Hospital of Athens, Athens, and the 4Department of Otolaryngology, Hippocration Hospital, Athens Medical School, Athens, Greece.
Abstract
Objectives: To investigate the topography of E-cadherin and its possible correlation with the histological phenotype of salivary gland tumours.
Material and methods: Archival formalin-fixed, paraffin-embedded sections of 54 benign and 56 malignant tumours and 24 samples of normal and inflamed salivary gland tissue were studied immunohistochemically using an Envision/horseraddish peroxidase (HRP) technique
Results: In normal and inflamed salivary gland samples, E-cadherin was expressed at the membrane of acinar, myoepithelial and ductal cells located at cell–cell contact points. Reduction and/or absence of E-cadherin was only observed in pleomorphic adenoma at the peripheral cells of the duct-like or island structures, or in the cells exhibiting plasmacytoid or stromal differentiation. Neoplastic epithelium in Warthin’s tumours and in myoepithelial and oncocytic adenomas was strongly positive. Furthermore, a weak to moderate loss of expression which was related to tissue tumour subtype was seen in malignant tumours such as: adenoid cystic carcinomas; polymorphous low-grade adenocarcinomas; acinic cell carcinomas; and mucoepidermoid low-grade, epithelial-myoepithelial, lymphoepithelial and squamous low-grade carcinomas. Moderate to extreme loss or alternative cytoplasmic non-functional expression were observed in cases of salivary ductal carcinoma, carcinosarcoma, myoepithelial carcinoma, oncocytic adenocarcinoma, unspecified adenocarcinoma and squamous high-grade carcinomas.
Conclusion: This study suggests a direct association of E-cadherin expression with neoplastic histologic phenotype, which is lost in the more undifferentiated and invasive epithelial salivary gland tumours.
18th Congress of International Federation of Otorhinolaryngological Societies, 25-30 June 2005, Rome, Italy
IMMUNOHISTOCHEMICAL DETECTION OF DESMOSOMAL CELL ADHESION MOLECULE DESMOGLEIN-2 (DSG-2) IN SALIVARY GLAND NEOPLASMS.
AUTHORS: 1 Andreadis DΑ, 1 Epivatianos Α, 3Nomikos Α, .2Mireas G, 1Poulopoulos Α, 2Vlahou S,1Antοniades, D, 2Papazoglou G, 2Christidis C, 3Barbatis C. .
AFFILIATION: 1Department of OraI Medicine and Maxillofacial Pathology, School of Dentistry, Aristotle University of Thessaloniki,2Department of Otorhinolaryngology and 3Department of Histopathology, Red Cross Hospital of Athens, Greece
IDEA: A comparative immunohistochemical study of the desmosomal cadherin Desmoglein-2 (Dsg-2) in normal, benign and malignant salivary glands.
METHOD: A total of 134 cases (24 normal, 54 benign, 36 malignant) were studied with the Envision – HRP immunohistochemical technique.
RESULTS: Dsg-2 is expressed along the basolateral surfaces of the epithelial cells of the normal acini and the entire ductal system with increased tensity at the basal aspect of the ductal epithelial cells. Warthin’s tumour and intercellular Dsg-2 expression but cytoplasmic localisation was diffuse in salivary ducts carcinomas, focal in acinic cell and adenoid cystic carcinomas and reduced in epithelial-myoepithelial, low grade polymorphous and basal cell adenocarcinomas with retention of the membranous distribution. Oncocytic, lymphoepithelial, mucoepidermoid and non-otherwise specified adenocarcinomas formed absent or limited cytoplasmic expression.
CONCLUSION: This is one of the very few studies on Dsg-2 expression in salivary glands and indicates quantitative and qualitative change in benign and malignant neoplasia and histological types. Further investigation is needed for assessing its clinical relevense.
18th Congress of International Federation of Otorhinolaryngological Societies, 25-30 June 2005, Rome, Italy
DUPLICATION OF THE THYROID GLAND
AUTHORS: Lefantzis D, Louverdis D,Dritsas G, Mireas G, Vlachou S, Plessas G, Papazoglou G
AFFILIATION: ORL department of the Red Cross Hospital of Athens.
IDEA: We present a case of ectopy and duplication of the thyroid gland
METHOD: The patient was a 40 years old man who was operated for multinodal goiter. The ectopy and duplication of the thyroid gland was a surgical finding during the routine thyroidectomy. More specifically there was a second thyroid gland with normal morphology but less than the half size, who was packed in between the infrahyoid muscles, immediately in front of the original thyroid
RESULTS: The operation completed when both the normal thyroid gland and the ectopic one were excised. No post-operated complications appeared.
CONCLUSION: Although duplication of thyroid gland is a rare finding all head and neck surgeons must be awared of it.
18th Congress of International Federation of Otorhinolaryngological Societies, 25-30 June 2005, Rome, Italy
EPITHELIAL – MYOEPITHELIAL CARCINOMA OF THE PAROTID GLAND
AUTHORS: 1Mireas G , 1 Louverdis D, 1 Christidis C, 2 Nomicos A. . 2Barbatis C 1Papazoglou G
AFFILIATION: 1Department of Otorhinolaryngology – Head and Neck Surgery and 2Department of Histopathology, Red Cross Hospital of Athens, Greece
IDEA: Two rare cases of epithelial–myoepithelial carcinomas of the parotid gland are presented
METHOD: The patients were females aged 44 and 49 yo, presented with a slowly growing mass of their left parotid gland, of 12 and 6 months duration respectively. The second patient also complained for slight pain in the parotid area. Preoperative CTs showed parotid masses.The patients were operated on and had an excision of the superficial lobe the first patient and of the deep lobe the second one. No patient underwent neck dissection.
RESULTS:Both operations had very good results with preservation of the facial nerve trunk and its main branches. The histological examination results were the following:
case 1: epithelial – myoepithelial carcinoma of 2 cm (max diam) with Ki67 ~5% and nuclear possitivity for p53<5%. Immunohistochemical study revealed: SMA (+), Bcl-2 (+), GFAP (+), EMA (+) and Mcyt (+).
case 2: epithelial – myoepithelial carcinoma of 1.8 cm (max diam) with Ki67 <2% and nuclear possitivity for p53~30%. Immunohistochemical study revealed: SMA (+), Bcl-2 (++), GFAP (++), S100(+).
The patients were not referred for radiotherapy or chemotherapy. A 4 years-follow up show no evidence of recurrency or distal metastasis.
CONCLUSION: Epithelial – myoepithelial carcinomas of the parotid gland are rare tumors with significant likelihood of recurrence 60% (3 years mean) and reveals metastatic disease in 9%. The surgical excision is the treatment of choise for this neoplasm and the follow up must continue for a period of two decades after operation.
18th Congress of International Federation of Otorhinolaryngological Societies, 25-30 June 2005, Rome, Italy
MALIGNANT ONCOCYTIC CARCINOMA OF THE PAROTID GLAND
AUTHORS: 1Vlachou S, 1Mireas G , 1 Triantos S, 1 Mavroidakos S, 2Barbatis C. . 1Papazoglou G
AFFILIATION:1Department of Otorhinolaryngology – Head and Neck Surgery and 2Department of Histopathology, Red Cross Hospital of Athens, Greece
IDEA: A rare case of a malignant oncocytic tumor of the parotid gland is reported
METHOD: The patient was a 82-years-old man, who presented with a rapidly growing and painful mass of the right parotid gland, of 5 months duration. The patient was operated on and had a right total parotidectomy with preservation of the facial nerve.
RESULTS: The histological examination revealed a malignant oncocytic tumor. The tumor recurred 2 months after the primary operation. The patient was referred for radiotherapy and chemotherapy but he unfortunately passed away 5 months later.
CONCLUSIONS: Tumors emerging from oncocytes are not frequent and the malignant variant is extremely rare, according to the literature. The purpose of this presentation is to contribute to the limited information regarding this rare entity.
18th Congress of International Federation of Otorhinolaryngological Societies, 25-30 June 2005, Rome, Italy
SARCOIDOSIS – ENT CLINICAL MANIFESTATIONS
AUTHORS 1SYMEONIDIS G 1MIREAS G, 1PAPADOPOULOS D, 1KAPRALOS V, 2VLACHOU S, 2 MAVROIDAKOS S, 1DEMEROUTIS I
AFFILIATION 1 251 HELLENIC AIR FORCES GENERAL HOSPITAL & V.A. ENT CLINIC 2 Department of Otorhinolaryngology – Head and Neck Surgery – Red Cross Hospital. Athens Greece.
IDEA Sarcoidosis is a chronic, multisystem granulomatous inflammatory disease of unknown etiology. Since its description in 1899 by Boeck, a remarkable number of potential causes have been implicated. The potential clinical manifestations of Sarcoidosis are numerous, mostly from the lower respiratory tract. We tried to find out how many ENT clinical manifestations exist due to Sarcoidosis.
METHOD We examined patients with known Sarcoidosis in whom their disease diagnosis had been confirmed by histologic examination. We performed a full ENT clinical examination, Opthalmology, Neurology and Laboratory tests.
RESULTS We examined 52 patients, from 1996 till 2004. A male preponderance of 29:23 was found. The average age of onset for women was higher than men (49yo vs 29yo). In 24 of the above patients, signs and symptoms of Head and Neck exothoracic Sarcoidosis occurred.
CONCLUSION ENT examination can be proved a useful tool for the diagnosis of Sarcoidosis, because ENT clinical manifestations are not so rare as it has been described till now.
18th Congress of International Federation of Otorhinolaryngological Societies, 25-30 June 2005, Rome, Italy
YELLOW NAILS SYNDROME-YNS AND SINUSITITS.
AUTHORS: Lefantzis D, Mireas G, Bshara B, Christidis C, Dritsas G, Mavroidakos S, Papazoglou G
AFFILIATION: ORL department of the Red Cross Hospital of Athens.
IDEA: A rare case of a patient with Yellow Nails Syndrome and sinusitis along with review of the literature is reported.
METHOD: The patient was a 40 years old woman who presented complaining for a persisting form of chronic sinusitis.
A full examination confirmed that she was suffered from the Yellow Nails Syndrome and its typical symptomatology.
The YNS is characterized by the triad of symptoms: scleronychia (yellow nails), peripheral lymphostasis and pleural effusion.
This rare syndrome is coupled with increased possibility of paranasal sinusitis (83%).
RESULTS: The treatment included corticosteroids and antibiotics with satisfied results.
CONCLUSION: An otolaryngologist is often the first medical doctor faced with the diagnosis and treatment of this syndrome,so he has to know about its features and treatment
18th Congress of International Federation of Otorhinolaryngological Societies, 25-30 June 2005, Rome, Italy
IMMUNOHISTOCHEMICAL DETECTION OF DESMOSOMAL CELL ADHESION MOLECULE DESMOGLEIN-2 (DSG-2) IN SALIVARY GLAND NEOPLASMS.
AUTHORS:1 Andreadis DΑ, 1 Epivatianos Α, 3Nomikos Α, 2Mireas G, 1Poulopoulos Α, 2Vlahou S,1Antοniades, D, 2Papazoglou G, 2Christidis C, 3Barbatis C. .
AFFILIATION: 1Department of OraI Medicine and Maxillofacial Pathology, School of Dentistry, Aristotle University of Thessaloniki,
2Department of Otorhinolaryngology and 3Department of Histopathology, Red Cross Hospital of Athens, Greece
IDEA:A comparative immunohistochemical study of the desmosomal cadherin Desmoglein-2 (Dsg-2) in normal, benign and malignant salivary glands.
METHOD:A total of 134 cases (24 normal, 54 benign, 36 malignant) were studied with the Envision – HRP immunohistochemical technique.
RESULTS:Dsg-2 is expressed along the basolateral surfaces of the epithelial cells of the normal acini and the entire ductal system with increased tensity at the basal aspect of the ductal epithelial cells. Warthin’s tumour and intercellular Dsg-2 expression but cytoplasmic localisation was diffuse in salivary ducts carcinomas, focal in acinic cell and adenoid cystic carcinomas and reduced in epithelial-myoepithelial, low grade polymorphous and basal cell adenocarcinomas with retention of the membranous distribution. Oncocytic, lymphoepithelial, mucoepidermoid and non-otherwise specified adenocarcinomas formed absent or limited cytoplasmic expression.
CONCLUSION: This is one of the very few studies on Dsg-2 expression in salivary glands and indicates quantitative and qualitative change in benign and malignant neoplasia and histological types. Further investigation is needed for assessing its clinical relevense.
5th European Congress of OtoRhinoLaryngology Head and Neck Surgery,September 11-16 2004, Rodos HellasGreece
ONCOGENE EXPRESSION IN HEAD AND NECK PARAGANGLIOMAS
MIREAS Georgios, MAVROIDAKOS Stavros, VLACHOU Stamatia, BARBATIS Calypso*, TSIKOY -PAPAFRAGOU Ekaterini*, PAPAZOGLOU Georgios
ENT Department, Red Cross Hospital Korgialenio-Benakio, Athens, Greece
*Department of Pathology, Red Cross Hospital Korgialenio-Benakio, Athens, Greece
Head and Neck Paragangliomas (PGL’S) are rare but true neuroendocrine neoplasia that may develop at many different sites with the commonest being the carotid body (CB-PGL’s) and the middle ear (ME-PGL’s).
A retrospective clinicopathological study was performed on 13 PGL’S of the Head and Neck, diagnosed and operated during the last 12 years in our Department: glomus tympanicum (7), carotid body tumors (4) and glomus jugulare (2). The patients were 4 males and 9 females, with a mean age of 52 years (range 37-69 years), followed up for a period of 1-12 years (Mean: 6 years). An immunohistochemical study was performed using the Envision/HRP method for the study of oncoprotein c-myc, the product of the antiapoptotic gene bcl-2 and the antigen of cell proliferation Ki-67.
There was diffuse cytoplasmic staining for all but two neoplasms for the c-myc protein. Bcl-2 expression was observed only focally and weakly in 5/13 cases, with a tendency for positivity for spindle cell type. Only in one large CB PGL (size 3 cm) showed 3% Ki67. All other cases were negative.
C-myc overexpression characterizes Head and Neck PGL’s. The low expression of bcl-2 and the almost undetectable proliferative rate may be relevant with the benign behavior of the tumors, as none had recurred.
- Da-Gong Wang, Aaros A.B. Barros D’ Sa, C. F. Johnston, K. D. Buchanan. Oncogene expression in carotid body tumors. Cancer, 1996, 77 (12): 2581-2586
- Pedro Filho, A. Rappaport, V.A.F. Alves, O.V.P. Denardin, J.A. Sobrinho, M.B. de Carvalho. Paragangliomas of the head and neck: clinical, morphological and immunohistochemical aspects. Sao Paolo Medical Journal, 2001,119 (3)
5th European Congress of OtoRhinoLaryngology Head and Neck Surgery,September 11-16 2004, Rodos HellasGreece
CAROTID BODY AND MIDDLE EAR PARAGANGLIOMAS. CLINICAL ASSESSMENT AND SURGICAL TREATMENT.
MAVROIDAKOS Stavros, MIREAS Georgios, VLACHOU Stamatia, LOUVERDIS Dionisios, TRIANTOS Stelios, PAPAZOGLOU Georgios
ENT Department, Red Cross Hospital Korgialenio-Benakio, Athens, Greece
Head and neck paragangliomas (PGL) are rare neuroendocrine tumors. They originate from various paraganglia, members of a complex of endocrine cells, the carotid body and the middle ear being the most common locations in the head and neck.
The clinical and pathologic features of 17 carotid body tumors and 20 middle ear tumors (15 glomus tympanicum and 5 glomus of the jugular bulb) diagnosed and operated in our Department were reviewed, as well as their surgical treatment. The patients were 15 males and 22 females, aged 37 to 69 years (mean: 54 yrs). Eighteen tumors presented on the left side and 19 on the right. Patients were followed up for 1-25 years (mean: 11 yrs). The initial symptoms and their duration, the extension of the tumor, the diagnostic evaluation undertaken along with the operative technique are presented and discussed.
The majority of glomus tympanicum (13/15) were operated through a transcanal approach and were submitted to a Farrior hypotympanotomy, and 2 were submitted to a radical mastoidectomy through a postauricular transmastoid approach. The glomus jugulare were operated through a combined mastoid-neck approach.
The carotid body tumors were approached through a lateral cervical incision at the carotid artery bifurcation level. In 7 cases we proceeded to ligation of the external carotid artery, in 3 patients to ligation of the internal carotid artery and by pass. One patient suffered a transient paresis of the XII nerve, while 1 patient developed hoarseness due to manipulation of the X nerve, which was satisfactorily recompenseted.
The surgical excision is the treatment of choice for head and neck PGL, with very good results. The only relative contraindication is the general condition of the patient may cause the application of an alternative treatment.
- Wang SJ, Wang MB, Barauskas TM, Calcaterra TC. Surgical management of carotid body Otolaryngol Head Neck Surg. 2000 Sep; 123(3):202-6tumors
- Plukker JT, Brongers EP, Vermey A, Krikke A, van den Dungen JJ. Outcome of surgical treatment for carotid body paraganglioma Br J Surg. 2001 Oct; 88(10):1382-6.
- Weber PC, Patel S. Jugulotympanic paragangliomas. Otolaryngol Clin North Am. 2001,34(6): 1231-40
5th European Congress of OtoRhinoLaryngology Head and Neck Surgery,September 11-16 2004, Rodos Hellas Greece
EXTENSIVE PLUNGING RANULA: A CASE REPORT
Authors: SIMEONIDIS S. George, GRIGORIADIS Kyriakos, PAPASTERGIOU Stavroula, MOIREAS George, DEMEROUTIS John.
Affiliation: 251 HELLENIC AIR FORCE HOSPITAL & V.A.
HEAD & NECK SURGERY DEPARTMENT.
Introduction: A plunging ranula is a mucous extravasation cyst of the sublingual gland, appearing as a swelling in the submental and submandibular regions.
Material & Method: We present a case of an extensive plunging ranula (sized 8X6 cm), involving multiple tissue spaces in a young woman 23 years old. The true extent of this lesion and its relationship to the surrounding anatomy, was well illustrated by CT scan. There was no intraoral appearance of the lesion.
Results: Ranula was managed surgically.
Conclusions: Plunging ranula is a very rare cystic lesion of the neck and must always be included in our differential diagnosis.
References: 1. Charnoff SK, Cart Barbara. Plunging Ranula: CT Diagnosis. Radiology 1986; 158:467-468.
- Coit WE, Ric Harnsberger H, Osborn G. Anne, Smoker RK Wendy, Stevens MH, Lufkin RB. Ranulas and Their Mimics: CT Evaluation. Radiology 1987; 163:211-216.
- De Vissher JGAM, Van Der Wal KGH, De Vogel PL. The Plunging Ranula. J Cranio-Max-Fac. Surg. 17(1989) 182-185.
- Karim Ali M, Chiancone G, Knox GW. Squamous Cell Carcinoma Arising in a Plunging Ranula. J Oral Maxillofac Surg 48:305-308, 1990.
- Lanlois NEI, BChir MB, Kolhe P. Plunging Ranula: A Case Report and a Literature Review. Hum Pathol 23:1306-1308.
- McClatchey KD, Appelblatt H Nancy, Zarbo RJ, Merrel DM. Plunging Ranula. Oral Surg. 57:408-412, 1984.
- Parekh D, Stewart M, Joseph C, Lawson HH. Plunging ranula: a report of three cases and reviw of the literature. Br J Surg 1987, Vol. 74, April, 307-309.
- Shelley MJ, Yeung KH, Bowley NB, Sneddon KJ. A rare case of an extensive plunging ranula: Discussion of imaging, diagnosis, and management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:743-6.
- Skouteris CA, Sotereanos GC. Plunging Ranula: Report of a Case. J Oral Maxillofac Surg 45:1068-1072, 1987.
- Takimoto T. Radiographic Technique for Preoperative Diagnosis of Plunging Ranula. J Oral Maxillofac Surg 49:659, 1991.
- Yoshimura Y, Obara S, Kondoh T, Naitoh SI. A Comparison of Three Methods Used for Treatment of Ranula. J Oral Maxillofac Surg 53:280-282, 1995.